Understanding HPV, Cervical Cancer, and Prevention: What you need to know!
Human Papillomavirus (HPV) is a common virus that primarily spreads through skin-to-skin sexual contact, causing various health concerns. What do you know about HPV? Maybe you have it, maybe you had it, and/or maybe your partner or partners have it – given how common HPV is, one or more of these things is probably true! It is estimated that more than 70% of sexually active Canadians will have a sexually transmitted HPV infection at some point in their lives (Government of Canada, 2020). Despite how common it is, there are still many myths and misinformation about what HPV is and what we can do about it. This blog aims to offer insights into HPV, cervical cancer screening, and important preventive actions, and challenge common myths about HPV.
What is Human Papillomavirus (HPV)?
As mentioned, HPV can be transmitted through intimate contact, often causing worry or embarrassment for individuals. However, it’s important to challenge the stigma surrounding HPV, as it is a widespread infection that is hard to prevent. Frequently, HPV infections present no noticeable symptoms, making it more difficult to detect.
Most HPV infections (9 out of 10) will resolve on their own within one to two years, primarily cleared by the immune system. However, persistent infections over a prolonged period can lead to various types of cancer (CDC, 2022).
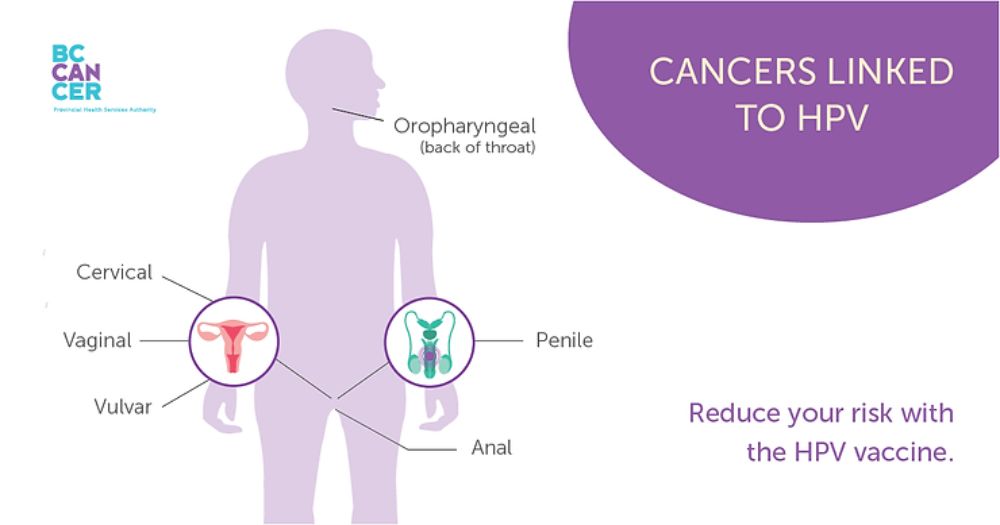
With over 100 types, approximately 40 affect genital, oral, or throat areas. These strains are categorized as “low-risk,” commonly resulting in genital warts, and “high-risk,” with the potential to cause various cancers (CDC, 2022). It’s important to note that having any type of HPV, including high-risk strains, does not guarantee the development of cancer, as the body often clears the infection without causing complications.

Prevalence of HPV in British Columbia:
Annually, thousands of cases related to HPV are reported in British Columbia, Canada. These include high-risk pre-cancerous changes to the cervix, cervical cancer, anal cancer, and cases of genital warts (BC Cancer Agency, 2023). According to BC Cancer:
- 6,000 individuals develop high-risk pre-cancerous changes to the cervix
- 200 individuals are diagnosed with cervical cancer, leading to 50 fatalities
- 110 people develop anal cancer, resulting in 20 deaths
- 5,500 individuals experience genital warts
Preventive Measures:
- Vaccination: HPV vaccines are recommended for preteens and individuals up to 26 years old, significantly reducing the risk of diseases caused by HPV, including various cancers (CDC, 2022).
- Cervical Cancer Screening: Routine screening for those assigned females at birth aged 21 to 65 years can prevent cervical cancer. Cervical screening tests detect abnormal cell changes, enabling early intervention (BC Cancer Agency, 2023).
- Safe Sexual Practices: Consistent condom and dental dam use and having open conversations with sexual partners about risks can lower the chances of contracting HPV and other sexually transmitted infections.

Who Should Get the HPV Vaccine?
The CDC recommends vaccination for:
- Preteens aged 11-12 years
- Individuals up to 26 years old who haven’t been vaccinated
- For adults 27-45 years old, vaccination decisions should be made after assessing their risk factors, although vaccination benefits are relatively lower in this age group.
How do I know if I have HPV?
Currently, there is no test to find out a person’s “HPV status” and there is no approved HPV test to find HPV in the mouth or throat. However, there are HPV tests that can screen for cervical cancer. Healthcare providers only use these tests for screening women, trans, and non-binary individuals assigned female at birth who are 30 years and older. HPV tests are typically not recommended to screen men, those assigned male at birth, adolescents, or those assigned female at birth who are under 30 years old.
Most people with HPV do not know they have the infection. They never develop symptoms or health problems from it. Some people find out they have HPV when they develop genital warts. Women, trans, and non-binary people assigned female at birth may find out they have HPV when they get an abnormal Pap test result (during cervical cancer screening). Others may only find out once they’ve developed more serious problems from HPV, such as cancers. All of these factors make diagnosing HPV challenging and those who suspect they may have it often feel anxious and uncertain about the outcome and what to do.
What are Genital Warts?
Genital warts are caused by certain strains of HPV. These warts typically appear on the genital or anal areas and are characterized by small, flesh-coloured, or gray growths or bumps. Genital warts can vary in size and may occur as a single wart or in clusters. They can be flat or raised, smooth or rough in texture, and might be painless or cause itching and discomfort. While they are generally not harmful and might disappear on their own, treatment options are available to manage symptoms and reduce the risk of spreading the infection. In addition, genital warts can prompt psychological distress and impact our genital body image.
What to Expect from a Pap?
Pap tests (cervical screening) can prompt anxiety and discomfort for many individuals leading to avoidance. This can put individuals at risk as Pap tests are essential in detecting abnormal cell changes. For those who may be avoiding a Pap test, we encourage you to find a healthcare provider you trust and to get the exam. Pap tests are conducted by various healthcare professionals like doctors, nurse practitioners, registered nurses, midwives, or naturopathic doctors. Pap tests are covered by MSP and are at no cost for those with MSP living in British Columbia.
During a Pap test, you’ll be asked to undress from the waist down and lie on a medical table, covering yourself with a gown or sheet provided. Your feet are placed in supports as the healthcare provider gently inserts a speculum into the vagina. Using a spatula or brush, they collect cervical cells. Just like any other medical exam, you have control the whole time and should let the provider know if you are feeling pain or discomfort.
The collected sample is sent to a lab for examination, and the results are shared with your healthcare provider. If any abnormal cells are detected, your provider will contact you for necessary follow-up appointments. It’s crucial to understand that an abnormal result does not necessarily indicate cancer, but attending follow-up appointments is essential.
BC Cancer recommends a regular cervical screening every three years as it plays a pivotal role in detecting and treating abnormal cells, reducing the risk of developing cervical cancer by up to 70%.
There are several myths and misconceptions surrounding HPV (Human Papillomavirus). Here are some common myths and the corresponding factual information:
- Myth 1: Only people with vulvas can get HPV
- Fact: Anyone can contract HPV through sexual contact. HPV infections are prevalent across sex and gender and can affect various areas, including the genitals, mouth, and throat.
- Myth 2: HPV only affects those who are promiscuous or have multiple sexual partners.
- Fact: HPV is highly common and easily transmitted through intimate skin-to-skin contact, including sexual activity. Even individuals who have had only one sexual partner in their lifetime can contract HPV.
- Myth 3: HPV always causes visible symptoms.
- Fact: Most HPV infections do not exhibit any symptoms, making it challenging for individuals to know if they are infected. Some types of HPV can cause visible symptoms such as genital warts, but many infections go unnoticed.
- Myth 4: Once you have HPV, you’ll always have it.
- Fact: In many cases, the immune system clears the HPV infection within one to two years. However, some people might have persistent infections that last longer, potentially leading to health issues. Most individuals clear the infection naturally without long-term consequences.
- Myth 5: HPV only leads to cervical cancer.
- Fact: While certain high-risk types of HPV can cause cervical cancer, they can also lead to other cancers such as vaginal, vulvar, penile, anal, and oropharyngeal cancers. Additionally, low-risk HPV strains can cause genital warts.
- Myth 6: HPV vaccines are only for young people.
- Fact: HPV vaccination is most effective when administered before exposure to the virus, ideally in preteens and young adults. However, vaccinations can still provide benefits for individuals up to age 45 who haven’t been previously vaccinated.
- Myth 7: Using condoms completely protects against HPV.
- Fact: While condoms and dental dams can reduce the risk of HPV transmission, it doesn’t offer complete protection. HPV can infect areas not covered by condoms, so the virus can still be transmitted through skin-to-skin contact.
It’s essential to address these myths with accurate information to encourage understanding, proper prevention, and vaccination against HPV. If you have specific concerns or questions about HPV, consulting healthcare professionals or reputable sources can provide accurate information and guidance.
PAP Screening at CAYA Health Centre
We know that not all healthcare experiences are the same. As much as we hope that all clinics offer trauma-informed and gender-affirming Pap care, we know that this is not the case. At CAYA Health Centre, we offer gentle Pap tests that are trauma-informed and gender-affirming. This means you have full control over how these procedures go. If you need a pause, or if it is uncomfortable, we can reschedule and continue the procedure another day. Our physicians will walk you through what to expect and the instruments they use. We also offer pre-medical support sessions with our registered clinical counsellors and registered pelvic floor physiotherapists. If you are feeling anxious or nervous about your appointment, please feel free to reach out! Learn more about our pre-medical support sessions here.

Book your Pap test today by calling us at 236-516-2292 or email us at info@cayahealthcentre.com.
Sources:
BC Cancer (2023.). The science. BC Cancer. https://www.bccancer.bc.ca/prevent/hpv/the-science
Centers for Disease Control and Prevention (2022). Genital HPV Infection – Basic Fact Sheet. https://www.cdc.gov/std/hpv/stdfact-hpv.htm
Government of Canada (2020.). Human papillomavirus (HPV). Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/human-papillomavirus-hpv.html
